Trigger Warning – Please be aware that this story contains discussion about miscarriage, ectopic pregnancy, issues with fertility, and medical mistreatment.
Pregnancy is often a time of joy and anticipation. For many, it marks the beginning of an exciting new chapter. But for me, it became a heartbreaking experience—one that tested my strength in ways I never imagined. I want to share my story in the hope that it helps others going through something similar feel less alone.
Getting Pregnant
When Oliver, my firstborn turned one, my husband, Tony, and I decided that we were ready to grow our family. I started taking ovulation tests the month of Ollie’s birthday, and soon enough, we were actively trying.

A few weeks later and I was testing like a madman, just like I had with Ollie, but every test was negative. One evening I had some pretty painful cramping and was hopeful that it might be implantation cramping, but then a few nights later I had a big bleed. Lasting for a few days, I assumed it was my period and I counted us out for that month. I was sad, but I already knew that it was unlikely that we’d get pregnant on our first go, and I knew that we’d just keep trying.
A couple weeks later, while I was putting Ollie to sleep, something happened. I was sitting in the rocking chair with him and spinning him around like he liked to do. My stomach flipped, and a bout nausea overcame me, which was very unusual. I got Ollie to sleep and I figured I would take a pregnancy test just in case. Surprise surprise, I got a very faint positive!
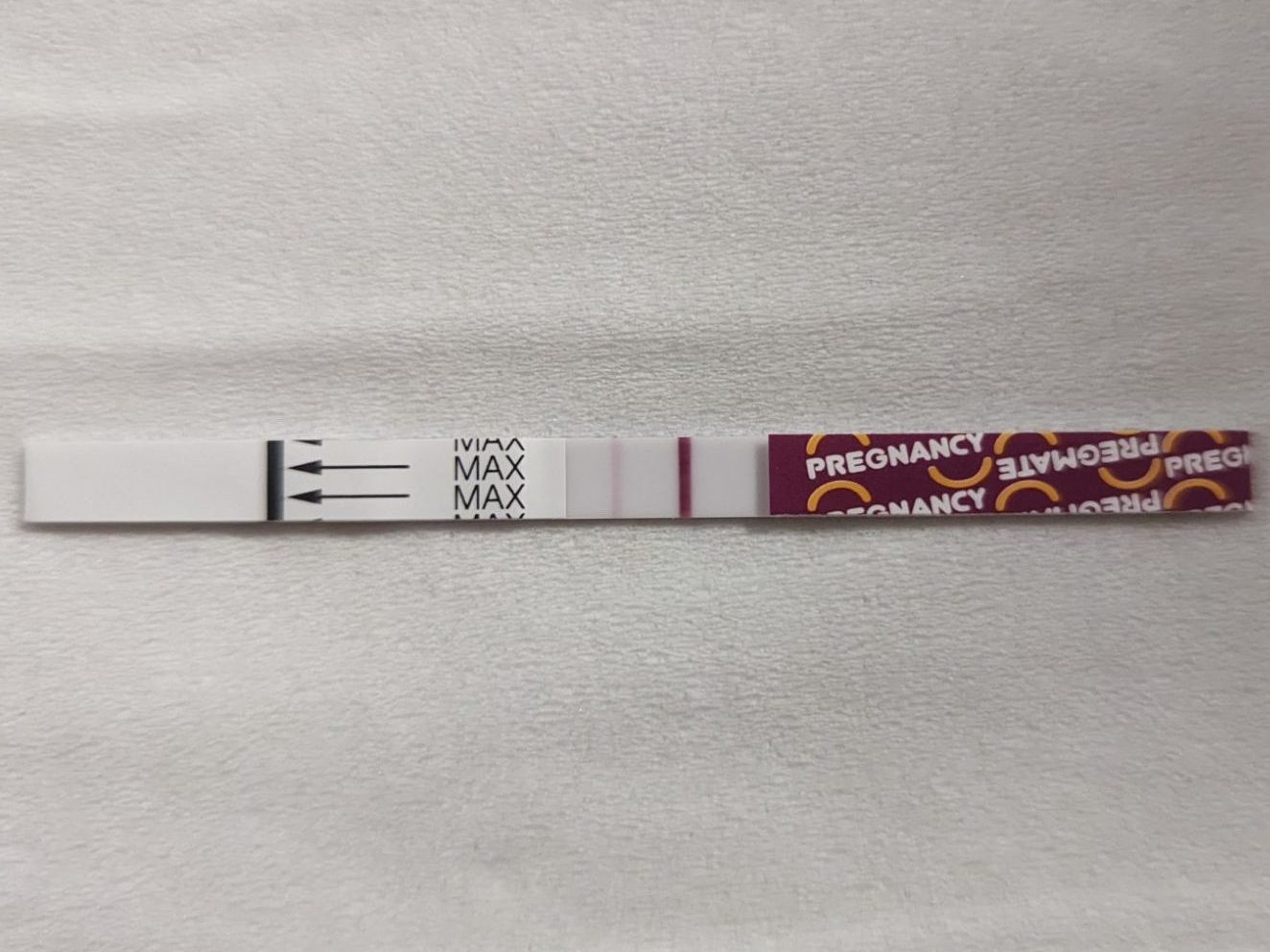
I ran downstairs and handed Tony the test. He looked and immediately saw the line, we were pregnant! Neither of us could believe that it had happened straight away, and we were also mind-blown that I was pregnant after thinking that I’d gotten my period. Over the coming days we told a handful of family and friends, excited about our news and the idea of growing our family.
Diagnosed Miscarraige
We went and saw our GP who did a beta HCG blood test, with a follow-up blood test a couple of days later. One evening I got a phone call from the doctor, who told me that my HCG had dropped in my second blood test, and advised that I was having a miscarriage. I was heartbroken. The doctor told me what to expect and wrote a referral for a follow-up blood test in case I didn’t start passing the pregnancy naturally by the end of the week. Tony and I cancelled our anniversary dinner planned for the following night, and he sent out a round of messages to the people we’d told, delivering the bad news.
A few days later, something felt off to me. Nothing physical, I just had a gut feeling that something wasn’t right. I hopped online and started looking for information about what to expect with a miscarriage. I saw somebody post about having an ectopic pregnancy that was diagnosed as a miscarriage, and that concerned me. Tony went out and bought me some more pregnancy tests so that I could take another one and compare the darkness of the test lines. The idea is that the higher your HCG levels are, the darker the test line will be. I knew that if I was truly having a miscarriage, the lines would become more faint, but when I took the test a very dark line immediately showed up.
More research unveiled another phenomenon called vanishing twin. This is when a twin (or more) pregnancy miscarries one of the foetuses. It can cause a temporary drop in HCG which then continues to rise. Tony and I grasped onto this concept and hoped that maybe we still had a viable pregnancy. We waited until the end of the week like the doctor had said and no symptoms of a miscarriage had appeared, so we went and completed the follow-up blood test. When we saw the doctor get the results, his eyes widened as he realized that my HCG had gone up again. This definitely wasn’t a miscarriage.
Dealing With Uncertainty
Tony and I were feeling very hopeful that this could be a case of vanishing twin. You know by the title of this post that it wasn’t, but we were trying to stay optimistic. Our doctor called a specialist to query why my HCG would have dropped and then risen again as he’d never seen this before. The specialist told him that this can be an indicator of an ectopic pregnancy, and advised that I needed to get scanned to find out where this pregnancy was.

Generally, with tubal ectopic pregnancies, there’s localized abdominal pain where the pregnancy is growing, but I didn’t have any pain, so I was hopeful that this wasn’t an ectopic. We presented to the hospital the following morning and told them what was going on and that I need it to be scanned. We are admitted into emergency and I was constantly asked about my pain levels which were zero. I had a very slight discomfort on the right side, which I told them, but nothing that was actually hurting.
After hours of waiting, I was finally scanned. The sonographer couldn’t find anything. I continued waiting to speak to a doctor. Obviously I was pregnant, otherwise I wouldn’t have rising HCG levels, but where the hell was his pregnancy? Was it somewhere it shouldn’t be? Or was it just too small to be seen?
During the wait, we Googled. While it was unlikely, it was not impossible for this to be a viable pregnancy. The rate of growth of my HCG was on the minimum end of what could be considered viable, and the fact that we couldn’t see the pregnancy at this stage, 7 weeks at the time, could be explained if I had ovulated very late, which I knew I had since I’d been testing. Tony and I were still hopeful that this could potentially be a viable pregnancy.
Finally, the doctor came to talk to me and told me that she thought it was an ectopic pregnancy, although they’d unable to locate it, and wanted to book me in for surgery to have it removed. She went on to tell me that my options were to have surgery to have my affected tube removed, or to be treated with a methotrexate injection into my bicep, which would essentially dissolve the pregnancy. She strongly advised against treating with methotrexate, as that would leave my tube scarred, increasing my chance of repeat ectopics in the future. She then gave me an anecdote about how in her time working as an OBGYN, she’s seen women treated with methotrexate having ectopic over ectopic because the embryos just keep getting caught in the scar tissue.
I told the doctor that I was uncomfortable having surgery if we didn’t even know where the pregnancy was and confirmed that it was definitely not viable. I queried as to how they would remove the pregnancy via surgery if they couldn’t even locate it on a scan. She told me that generally when they open a woman up to operate for an ectopic, it’s pretty obvious where the pregnancy is. I told her that I was still uncomfortable consenting to a surgery before we ruled out a viable pregnancy and were able to locate it. That’s when she left and returned with the senior OBGYN. I requested to go home and come back in 48 hours to rescan and reiterated that I wasn’t comfortable having surgery until the pregnancy had been located. He told me that because I lived close, and I wasn’t in any pain, that it would be fine for me to do that, so off we went.
As promised, 48 hours later I returned to have another scan and blood test. My HCG was still rising, but this time the sonographer wouldn’t let me see the screen while she scanned and wouldn’t tell me any information about what she was seeing despite my multiple requests to know. Tony and I then sat in a waiting room for 3 hours while we waited to speak to a doctor to find out if we had a viable pregnancy or if they were able to locate it. This 3-hour wait was really hard, I remember my heart rate was through the roof with anxiety.
Diagnosed Ectopic Pregnancy
We were finally called in to see a doctor, which happened to be the same doctor that had originally advised me to have surgery. She sat us down and said, “We think we found the pregnancy in the left tube, so we’d like to book you in for surgery and remove it”.
My response was, “You think you found the pregnancy, or you have found the pregnancy? Because I’m uncomfortable having a surgery unless we have actually confirmed the location of it.” I then went on to explain why Tony and I were optimistic about the possibility of it being a viable pregnancy. I explained that I understood the chances were that it was an ectopic but that until we could find it, I didn’t want to have surgery.
That’s when the doctor responded with, “This is the pregnancy, there’s nothing else that it could be.” I told her that if they were sure that they’d found it, then I would consent to the surgery, but if they opened me up and it wasn’t obvious that I had an ectopic, then I didn’t want them to remove anything. She told me that that was fine and that if they weren’t sure in the procedure, then they wouldn’t remove my tube.

They wanted to keep me overnight in the hospital and then have the surgery the following day, but living only 5 minutes from there, I asked if it would be okay for me to go home for the night and come back in the morning. That way I could still be with my firstborn overnight. I advise that I still wasn’t having any pain or bleeding which are indicators of a more urgent ectopic. She allowed it and we headed home. Unfortunately that evening I started spotting so I headed straight back to the hospital and stayed the night.
Surgery to Remove Ectopic Pregnancy
My surgery was continuously pushed and what was meant to be an early morning surgery became afternoon. I remember they got me into a gown and on a bed, and then left me in a hallway by myself for at least an hour with no phone or anyone else to talk to to keep myself busy. I just laid there, alone, waiting to have my pregnancy taken out of me, my mind racing and my heart breaking.
Eventually I was wheeled into pre-op where a cannula was put in my hand. I remember they couldn’t find a vein and had to use an ultrasound on to get it in. I had to wait in pre-op for a while because the operating room was being used for a c-section. The surgeon came in and met me and told me that he would be taking some photos while he was inside. During this, I could hear the baby that had just been born on the other side of the doors start crying.
I was wheeled into the operating room, and the anaesthetist told me that she was going to administer some drugs through the cannula that would make me feel drunk. She was exactly right, I felt drunk and soon I was unconscious.
The next thing I remember, I started to wake up. Before I even opened my eyes tears were falling from them. My pregnancy was gone and my heart was broken. I couldn’t stop thinking about the little baby that I was meant to be growing, who wasn’t with me anymore. I was incredibly groggy while I woke up further but I was still crying. The surgeon came to see me and told me that they’d taken my tube and that they had taken photos, and then he left.
Soon I was taken back to the maternity ward where I would recover. While I was in there I could hear the babies that had just been born, crying. I felt broken, like a piece of me was missing.
I was discharged that evening and went home. Having Ollie at home, shining so brightly, helped me so much. If I didn’t have him being his happy little self, I just can’t imagine how sad the house would have been.
Life went on. I was still heartbroken, but I was trying to take the time that I needed to grieve, and to physically heal.
Medical Mismanagement Revealed
Two weeks later, on the day before Good Friday, Tony was in Sydney for a work day trip. I received a phone call from the hospital asking me to come back and do a follow-up beta HCG blood test. I thought it was weird, but I figured that it must be routine, so I packed up Ollie and headed to the hospital. My blood was taken and I went home. A couple of hours later I was called by the hospital again and advised that I was very much still pregnant and that I needed to return for a scan. I was now 9 weeks pregnant according to my last menstrual period.
Tony was on his way home from Sydney and waiting at the airport for his flight. I called my sister to help me manage Oliver while I had my scan. Her and her husband met us at the hospital, and she came in with me for the scan while her husband entertained Ollie in the waiting room. The sonographer didn’t say much, and didn’t let me watch the scan, but when I asked if she was seeing anything, she simply told me that she was seeing a “not alive pregnancy on the right side”. After my scan I was sent back up to the labour and delivery ward where I waited to speak to an obstetrician.
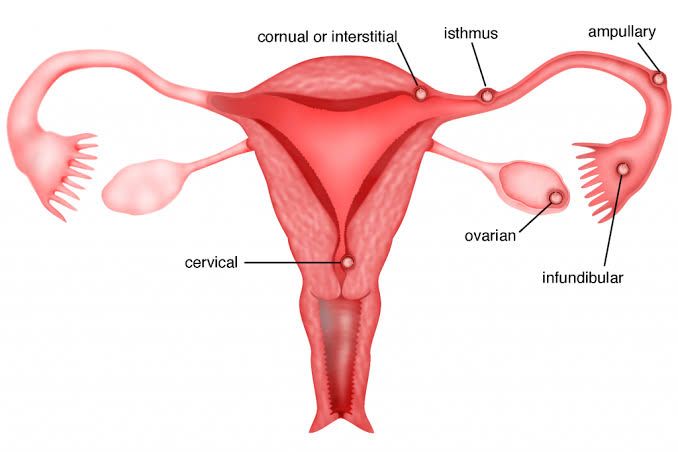
Finally, I was called in to a delivery room. I was told that when my tube was removed, it was sent off to be tested, which came back as not containing a pregnancy, hence the follow-up blood test. I was then advised that the scan had revealed I had what is called a cornual ectopic, which is where the embryo implants in the uterus but in the upper area where the fallopian tube enters the uterus. This is still a non-viable pregnancy, as the uterus in this location is unable to stretch as much as required to carry to term. The doctor told me that this is a much more complicated type of ectopic to manage. He told me they weren’t confident at that hospital that if something went wrong in surgery, they’d be able to save my life. I let him know that I also was not confident in that hospital, and so I was transferring to a larger hospital. I ended up driving myself there after taking Oliver home where my sister and her husband looked after him.
Methotrexate Treatment
Tony managed to meet me at the other hospital just as I parked. We were checked into the early pregnancy assessment unit. We waited there for upwards of 6 hours. Late that night I was finally seen and scanned, and for the first time through this ordeal, the sonographer let me see the scan while it happened. What I saw was a large mass. The fact that it wasn’t in the shape of a foetus, and didn’t have a heartbeat I actually found helpful. It made it hurt a little bit less.
By this point it was the middle of the night. The hospital sent Tony home, and I was taken to the maternity ward to try and get some sleep. The following morning an obstetrician came in to speak to me. He told me that there were two options of treatment. One was surgery, which with a cornual ectopic was basically a pizza slice out of my uterus, and would mean that any future births would always have to be c-sections. It also meant that I would definitely become infertile and unable to get pregnant without IVF. The other option was to treat with a much higher dose of methotrexate than usual, but he was an unsure if I would be a suitable candidate for this method of treatment because the pregnancy was so far along and my HCG was so high. Being treated with methotrexate would mean that I still had the option of having a VBAC (vaginal birth after c-section) in the future, and could potentially mean that I retained fertility, however, I was advised that this was unlikely.

We decided to do another blood test to see what was going on with my HCG levels. I was told that if it had gone up from the previous day’s test, I would be looking at surgery, but if by some miracle it had decreased, then I could be a candidate for methotrexate. My blood was drawn and then I waited. Finally, I was given the great news that it had decreased by nearly 30% and I chose to be treated with methotrexate.
I was transferred to the cancer hospice ward for treatment. By this time it was the following evening from when I had been admitted into this hospital. I was put in a room and waited, again. A nurse came in in full protective gear to administer the treatment. I was given a high dose of 200 mL intravenously over the course of 5 minutes, and then I was given an additional (I believe, my memory isn’t perfect) 500 mL in a drip over the next 12 hours. This treatment made me really nauseous and I was given some anti-nausea tablets to help combat it.

Being treated with methotrexate leaves patients immunocompromised, and it also is a danger to other people in their household. I was told that for 7 days I couldn’t share any bodily fluids with anyone. That meant that I couldn’t kiss my husband or my baby, and it meant that I couldn’t breastfeed Ollie in this time which broke my heart.
After my treatment was completed I was moved back to the maternity ward to recover. I was nauseous and just felt like crap overall. Once again, I was dealing with the loss of my pregnancy while I heard the other women and babies in the unit. I understand that this unit is where the professionals that handle these situations work, but putting women who are in the midst of dealing with pregnancy losses like this next to women with live babies feels extremely inconsiderate.
I spent the entire Easter weekend in the hospital. Finally, I was discharged and sent home. I felt like I hadn’t had the proper time to grieve my pregnancy loss before I was dealing with it again. It felt so unfair that I had to do this twice, and on top of that now there was the possibility of infertility.
Meeting With the Original Treating Hospital
I was invited to return to the original treating hospital for a meeting where I could ask any questions that I had. I booked in a meeting and Tony and I attended together. We met with the senior OBGYN that had allowed me to return home after my first presentation to hospital. He basically told us that it was a terrible thing to have had my healthy tube removed, but that that was just a thing that can happen. It felt very, sorry not sorry.
I asked to see the photos that had been taken during the surgery. First, he said that there weren’t any photos, but I told him that the surgeon had told me that he’d taken some and that I wanted to see them. He took a really long time trying to find them in the system, but Tony and I waited patiently. Eventually they were found. It was clear that there was some swelling in the tube that was removed, but it certainly wasn’t localized swollen like is seen in tubal ectopic pregnancies. It’s also worth noting that tubal swelling can happen with pregnancy hormones running through the body, so generalized swelling of tubes definitely doesn’t always mean an ectopic, or even that there’s something wrong.
Most interestingly, there was very clearly a cyst right next to my tube. This is obviously what was seen on the scan, and my mind was baffled as to why this connection wasn’t made during surgery. We asked the doctor, looking at those photos, did he think that it looked like there was a pregnancy in my tube. His first response was no, and then when Tony asked him to confirm that he didn’t think that that was a pregnancy, he backtracked and said that it was hard to tell.
Sensing that we weren’t satisfied with the hospital ‘s explanation for why this had happened to me, he told us that we could submit a complaint to the patient liaison if we liked. Leaving that meeting, I realized how much I was hoping to see a very swollen tube. Something that I could look at and say, well that looks like an ectopic. It would mean that, while the outcome was still the same, the removal of my tube at least made sense. Instead I came out feeling like the people doing my surgery just couldn’t be bothered to think about me as a real human, and instead I was just on the patient conveyor belt, getting pushed through the system as quickly as possible.
As soon as we were home, I typed up my complaint and contacted the hospital’s patient liaison to submit it. I was advised that the hospital would be opening an independent investigation into what had happened, and that I would be advised of the results. I asked how long these investigations tend to take, not to put on any pressure, I just honestly didn’t know how long these things took, and I was advised approximately 3 months.
Fertility Testing
We had to wait about 6 months before we could complete what’s called a hyfosy scan which is when they inject a dye foam into the uterus and use ultrasound to check for tubal patency (if your tubes are open or blocked).
The scan was incredibly unpleasant. I think normally when you have patent (open) tubes, as the foam is injected, it flows out of the tubes and into the rest of your body to be absorbed. But for me, there was nowhere for the foam to go, so pressure just built up in my uterus. It hurt as much as being in labor with my first born did, and Tony even told me that I looked like I was in labor again. Sure enough, the heartbreaking news that my remaining tube is blocked came. I knew this was a real possibility, but it just felt like blow after blow.
Hospital Investigation
Nine months after my ectopic pregnancy we were called to return to the original treating hospital to be advised of the outcome of the investigation. Arriving at the hospital, prepared to go in and discuss everything that had happened, and face the people in charge of the hospital that had turned my life upside down, I nearly had a panic attack. I was fighting back tears walking through the parking lot. We arrived on time for our meeting, but the hospital wasn’t ready and we were left waiting, again.
Finally, we were taken to a meeting room where we sat down with the head of obstetrics and the head of the hospital. Contrary to what we had been told, The investigation was not complete and this meeting was not to advise us of the outcome, but instead to get our side of the story.
I told my story in great detail, crying through the entire thing. The hospital staff in the room was empathetic, and for the first time I felt as though I was actually being heard, and my hurt was being understood. Not much more came from that meeting, there was no information to give us, so Tony and I went home.
A few months later, about a year after I was treated, we were called back to the hospital. This time the investigation had actually been completed. While the investigation didn’t clearly state that the hospital was at fault, it did recognize that there was undue time related pressure placed on me to be treated, and that the diagnosis of my ectopic should have taken the time to actually locate the pregnancy definitively prior to treating.
The hospital told me that they would use my scenario as an example when speaking to their departments about best practice. They also told me that they’re developing interunit meetings, to allow learnings from any unit, to help all units improve.
Mental Health Challenges
My mind still feels like a jumbled mess when I think about the effects that this has had on me. I had to experience a pregnancy loss twice for the same pregnancy, I was left with an ectopic pregnancy until 10 weeks pregnant, which if it had a ruptured could have killed me. I wasn’t listened to at the hospital about my concerns regarding removing an unaffected tube and I felt rushed through the system. I had my fertility stolen from me.
This ordeal affected myself, and my husband, greatly. It made me depressed, gave me regular panic attacks and hugely heightened anxiety, and it left me with a great deal of mistrust for medical professionals in the obstetrics sector. I learned that healing isn’t linear. Some days, I felt okay. Other days, I was really struggling. I’ve been to counseling and therapy, which has helped, but it’s definitely still something I’m dealing with.
To the people in my life that were there for me and supported me through this, thank you, I am forever grateful to you.
That’s my story. It’s a story of loss, heartbreak, and let downs. There’s no happy ending to this story. That’s just the end, because some things in life don’t have happy endings.
Breaking the Silence
If you’re going through an ectopic pregnancy, please know that you are not alone. Your pain is real, your grief is valid, and you deserve support. There is no right or wrong way to heal—just take it one day at a time.
Pregnancy loss, isn’t talked about enough, but by sharing our stories, we can break the silence. We can support each other and remind ourselves that even in our darkest moments, we are not alone.
To anyone who has experienced an ectopic pregnancy: I see you, I honour your pain, and I stand with you.
x Laura


Beautiful written love my heart broke all over again reading this. Thank you for sharing ♥️
LikeLiked by 1 person
Thank you ❤️
LikeLike
Laura, So sorry to read this. Thank you for having the courage to write it.
LikeLiked by 1 person
Thanks so much Michael ❤️
LikeLike